A full medical history and thorough physical exam are required for the initial clinic visit. The circumferential differentiation between the affected and unaffected limbs (in unilateral disease) will be the focus, and measured comprehensively during the physical exam. Based on the findings, diagnosis and subsequent treatment options will be suggested and referred by Dr. Cheng’s lymphedema grading system.
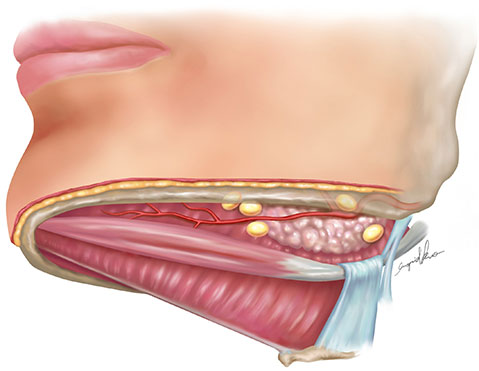
Accurate diagnosis and appropriate staging assessment are fundamental to the successful treatment of lymphedema. The conventional treatment methods often require the use of antibiotics, massage, and complex decongestive therapy including compression garments and bandages. Innovative surgical treatments have been emerging rapidly in the past 10 years, and the ground breaking vascularized submental lymph node (VSLN) or vascularized groin lymph node (VGLN) flap transfer to distal recipient site that invented by Dr. Cheng create a natural physiologic drainage conduit to alter excess lymphatic fluid buildup and revert side effects like those of tissue fibrosis and skin swelling. Dr. Cheng’s surgical treatment outcomes show significant improvements in the circumferential reduction rates of the affected limb circumference without the use of compression garments.
 Mean 7.2 lymph nodes at MRI study. 61% lymph nodes located in central 2 quarters Mean 7.2 lymph nodes at MRI study. 61% lymph nodes located in central 2 quarters |
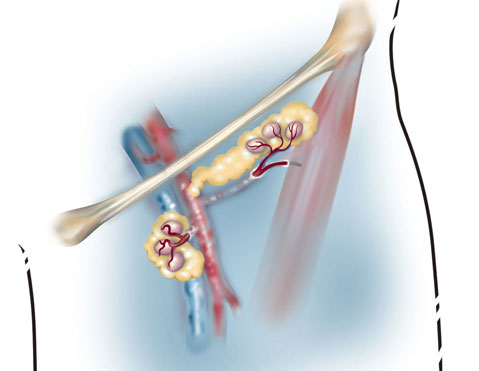 Mean 6.2 lymph nodes. Mean 6.2 lymph nodes. |
|
|---|---|---|
| Candidates |
|
|
| Procedures | Transfer the submental lymph node flap to the wrist with maximal functional and cosmetic recovery
Tmaximal lymphatic drainage with the “Pump” effect, catchment effect, and gravity effect. |
Transfer the vascularized groin lymph node flap to the wrist with maximal functional recovery
maximal lymphatic drainage with the “Pump” effect, catchment effect, and gravity effect. The occurrence of donor site lymphedema is very low (<3%) and it can be avoided by using the technique of reverse lymphatic mapping of combination Technetium-99 and indocyanine green lymphography |
| Results | Vascularized lymph node flap transfer was significantly superior to lymphovenous anastomosis or complete decongestive therapy in terms of improvements in the circumferential difference, reduction rate and episodes of cellulitis. Microsurgical treatment of lymphedema with VLN transfer procedures effectively decrease limb circumference. This improvement is mirrored by improvements in patient-reported outcomes and quality of life. These changes can be observed as soon as 1 month postoperatively, and continued steady improvement can be expected. |
Microsurgical treatment of lymphedema with VLN transfer procedures effectively decrease limb circumference. This improvement is mirrored by improvements in patient-reported outcomes and quality of life. These changes can be observed as soon as 1 month postoperatively, and continued steady improvement can be expected. |
| Quality of Life | As for the Lymph Quality of life (QoL) questionnaire (1- 10, the higher the better), the overall Lymph QoL was increased from 2.2 to 7.4 for upper limb lymphedema; and increased from 3.2 to 7 for lower limb lymphedema at 12- months of follow-up. | As for the Lymph Quality of life (QoL) questionnaire (1- 10, the higher the better), the overall Lymph QoL was increased from 2.2 to 7.4 for upper limb lymphedema |
